Expert Help for OCD
Take Your Life Back from OCD
Offering expert treatment for all types of OCD, including unwanted obsessional thoughts. Our OCD treatment program is typically 10 weeks. We offer twice-weekly sessions, groups, and intensive programs. Intensive program can be in person or online. Low cost options available. Contact us...
Behavioral Wellness Clinic
392 Merrow Rd, Suite E,
Tolland, CT 06084
Office: (860) 830-7838
OCDTYPES
Obsessive-compulsive disorder comes in many forms
Hair-Pulling Disorder (Trichotillomania)
The New England OCD Institute Explains Hair-Pulling Disorder
Symptoms of Hair-Pulling Disorder
People with Hair-Pulling Disorder (also called trichotillomania or TTM) have strong urges to pull hair from their scalp, eyelashes, eyebrows, pubic area, or elsewhere on their bodies. People with Hair-Pulling Disorder may pull out thousands of strands of hair every month, anywhere from 10 to 500 hairs a day. Most people with Hair-Pulling Disorder feel a great deal of shame around their condition, regardless of the location of the hair pulling.
Hair-Pulling Disorder is not the same as Obsessive-Compulsive Disorder (OCD), although they both involve repetitive behaviors and some people have both conditions. Hair-Pulling Disorder is considered an OCD Related Disorder, although it has also been conceptualized as an impulse control disorder. The typical onset of Hair-Pulling Disorder is between the ages of 9-13, although this behavior had been observed in small children and even infants. Hair-Pulling Disorder can be treated with behavioral techniques including habit-reversal training to better control hair pulling, often in concert with other techniques designed to help decrease the urge to pull.
Why do people compulsively pull their hair?
Hair-Pulling Disorder involves repetitive hair pulling, resulting in noticeable hair loss. People suffering from Hair-Pulling Disorder often report experiencing a mounting tension or urge to pull and a sense of relief or pleasure after pulling. The scalp is the most common site in adults and in youth, however pulling may occur at any hair site including eyebrows, eyelashes, legs, arms and pubic areas. However, sometimes people pull hair without awareness. Pulling may be either focused and intentional in response to emotional cues (such as stress or relationship problems), or it may occur without the person realizing, such as during sedentary tasks (i.e., watching T.V. or reading).

There are few large-scale studies on the prevalence of Hair-Pulling Disorder or Trichotillomania, although one study conducted by the University of Pennsylvania faculty, in collaboration with colleagues at the University of Delaware, suggested that about 1 in 50 college students report clinically relevant hair pulling and skin picking. Most recent estimates place hair-pulling at 0.6-1.0%.
Is compulsive hair pulling harmful?
Hair-Pulling Disorder can be harmful because it can interfere with social relationships, making people unwilling to go out in public or start dating relationships. This is because chronic hair pulling can result in embarrassing bald spots or complete loss of hair. Ongoing pulling can cause weakening of the root bed, resulting in a permanent change of hair texture or permanent bald spots. Some people ingest their hair, which can cause intestinal problems or even the formation of dangerous trichobezoars that get stuck in the digestive system and require medical intervention to resolve.
Treatment for Hair-Pulling Disorder
Several adult studies and more recent child and adolescent studies highlight the social and functional problems associated with chronic hair-pulling. The best treatment is Habit Reversal Therapy (HRT), a form of behavioral therapy proven to effectively treat Hair-Pulling Disorder. This treatment retrains the client's response to the urge or sensation to pull their hair. The program begins by developing awareness of the pulling habit itself. Many people suffering from Hair-Pulling Disorder experience an urge to pull or a tense sensation just before pulling. The initial component of the program aims to bring this preliminary urge or sensation to consciousness. This is often accomplished through self-monitoring and record keeping. Clients may even be asked to save the hair (e.g., put it in an envelope) and bring it to session to monitor progress, if they are willing to do so.
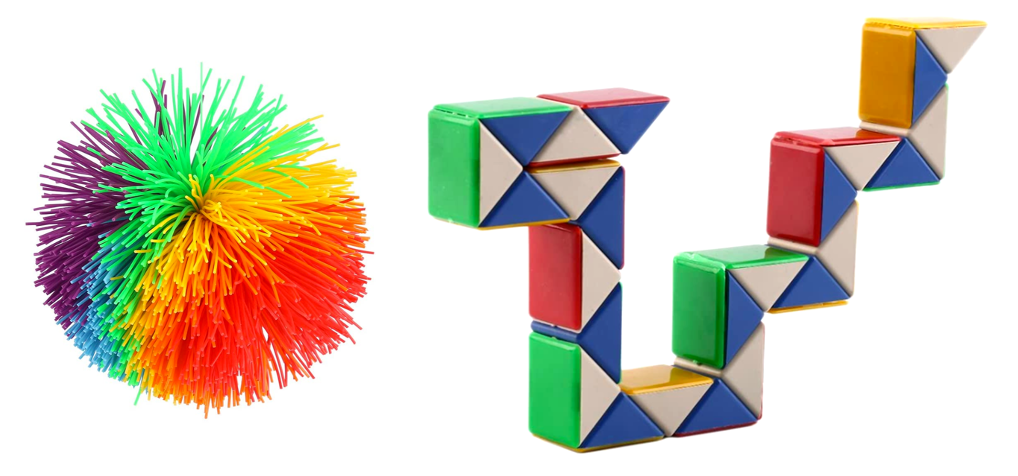
Muscle relaxation and diaphragmatic breathing techniques may also also taught to reduce the level of bodily sensation and tension that may lead to pulling. Most importantly, the patient develops a "competing response" or alternative behavior that is incompatible with pulling (i.e., make a fist or use a fidget toy). The competing response must be both behavioral and observable, using the part of the body that is involved in the pulling (generally the forefinger and thumb). This activity is performed at the first indication of an urge and conducted until after the urge subsides (about 60 seconds). This response is a replacement behavior, training the person to do something different in response to the urge. The goal of treatment is to become aware of triggers and situations connected to pulling and gradually create new connections in the brain with a non-destructive behavior. Often a support person, such as a partner or parent, can be helpful in bringing about change by encouraging the person when things get tough or praising them when they make use of their competing responses. Therapists can work with loved ones to enable them to support the person with hair-pulling disorder in the best way possible.
The three keys of Habit Reversal Therapy:
- Awareness of the Urge to Pull
- Competing Response Training
- Social Support Training
Habit Reversal Therapy is sometimes combined with Acceptance and Commitment Therapy (ACT). This approach helps clients focus on their goals and values to help motivate them to change. In ACT, clients learn to recognize the urge to pull and accept that they feel may feel temporarily uncomfortable when they resist pulling. Clients adopt a willingness to resist, and they also learn to show self-compassion when they do pull and address feelings of shame around their behavior.
Treatment for Hair-Pulling Disorder is typically short term. The client and therapist meet weekly for 8 weeks, and then every other week thereafter until the hair pulling is resolved.
Some Items to Combat Hair-Pulling Disorder
Fidget toys can be an important tool to help combat the urges to pull hair. Below are some suggested items that can help.

Nuts and seeds with the shell on can be a great way to keep hands busy and away from hair. If hair-pulling occurs at night, sleeping with gloves or mittens on will also help. People with Hair-Pulling Disorder should try several of these strategies and stick with the ones that work the best.


